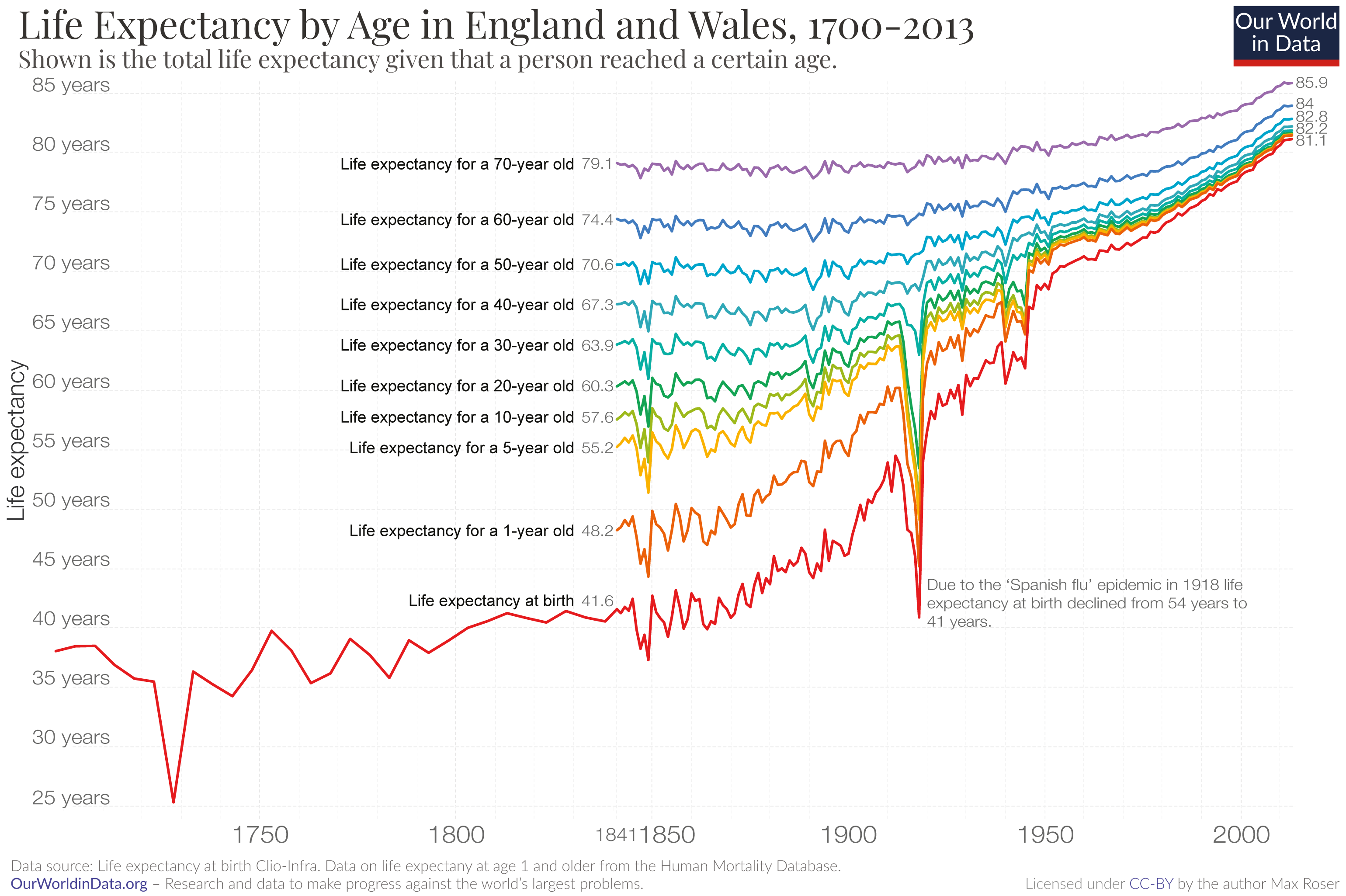
In the last 150 years the world has seen an unprecedented improvement in health. The visualization shows that in many countries life expectancy, which measures the average age of death, doubled from around 40 years or less to more than 80 years. This was not just an achievement across the countries shown here; life expectancy has doubled in all regions of the world.
What also stands out is how abrupt and damning negative health events can be. Most striking is the large, sudden decline of life expectancy in 1918, caused by an unusually deadly influenza pandemic that became known as the ‘Spanish flu’.
To make sense of the fact life expectancy declined so abruptly, one has to keep in mind what it measures. Period life expectancy, which is the precise name for this measure, captures the mortality in one particular year. It summarizes the mortality in a particular year by calculating the average age of death of a hypothetical cohort of people for which that year’s mortality pattern would remain constant throughout their entire lifetimes.
This influenza outbreak wasn’t restricted to Spain and it didn’t even originate there. Recent genetic research suggests that the strain emerged a few years earlier, around 1915, but did not take off until later on. The earliest recorded outbreak was in Kansas in the United States in 1918.1
But it was named as such because Spain was neutral in the First World War (1914-18), which meant it was free to report on the severity of the pandemic, while countries that were fighting tried to suppress reports on how the influenza impacted their population to maintain morale and not appear weakened in the eyes of the enemies. Since it is very valuable to speak openly about the threat of an infectious disease I think Spain should be proud that it was not like other countries at that time.
The virus spread rapidly and eventually reached all parts of the world: the epidemic became a pandemic.2 Even in a much less-connected world the virus eventually reached extremely remote places such as the Alaskan wilderness and Samoa in the middle of the Pacific islands. In these remote places the mortality rate was often particularly high.3
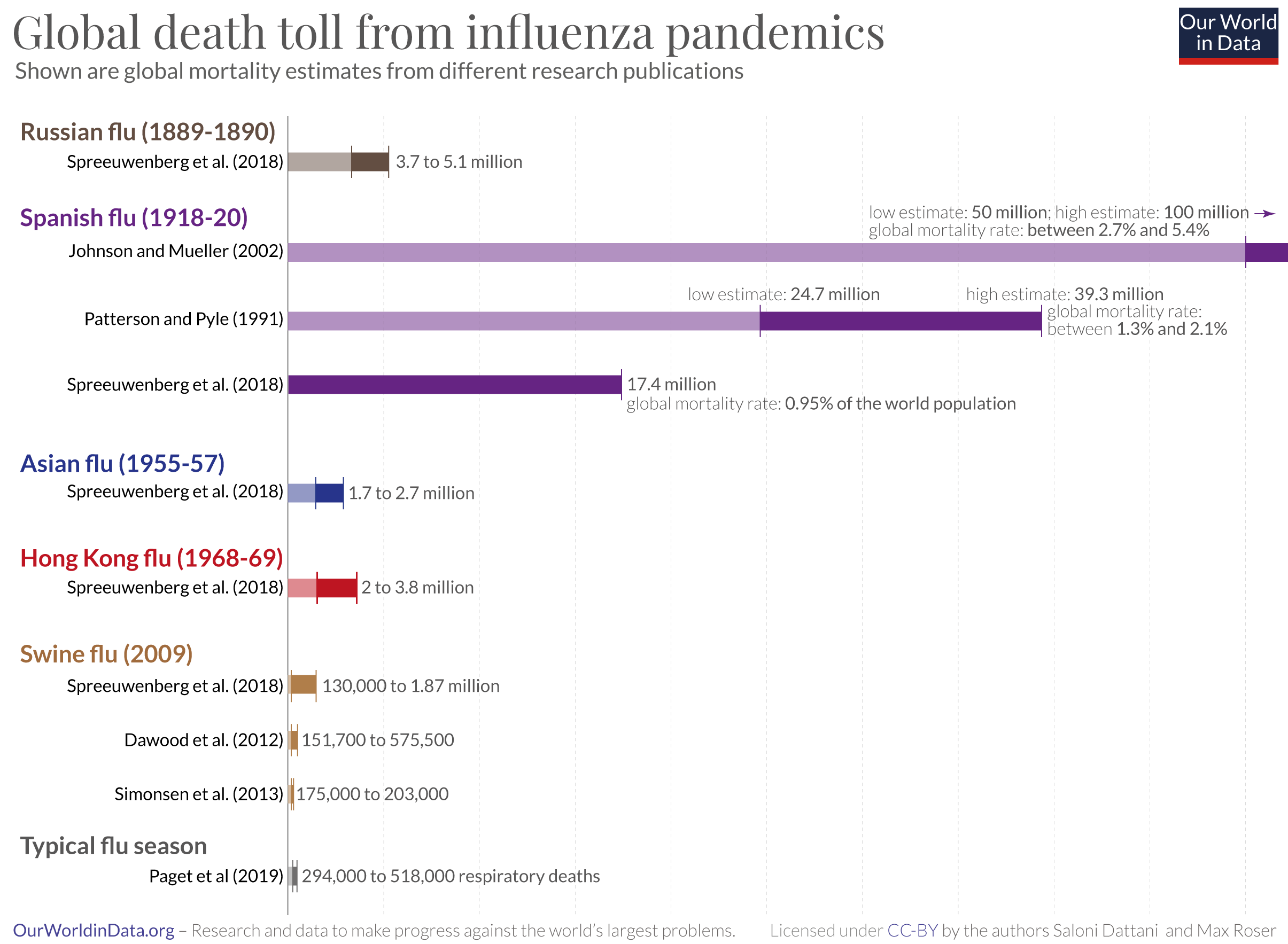
The global death count of the flu today:
To have a context for the severity of influenza pandemics it might be helpful to know the death count of a typical flu season. Current estimates for the annual number of deaths from influenza are around 400,000 deaths per year. Paget et al (2019) suggest an average of 389,000 with an uncertainty range 294,000 from 518,000.4 This means that in recent years the flu was responsible for the death of 0.005% of the world population.5 Even in comparison to the low estimate for the death count of the Spanish flu (17.4 million) this pandemic, more than a century ago, caused a death rate that was 182-times higher than today’s baseline.
Global deaths of the Spanish flu
Several research teams have worked on the difficult problem of reconstructing the global health impact of the Spanish flu.
The visualization here shows the available estimates from the different research publications discussed in the following. The range of published estimates for the Spanish flu is particularly wide.
The widely cited study by Johnson and Mueller (2002) arrives at a very high estimate of at least 50 million global deaths. But the authors suggest that this could be an underestimation and that the true death toll was as high as 100 million.6
Patterson and Pyle (1991) estimated that between 24.7 and 39.3 million died from the pandemic.7
The more recent study by Spreeuwenberg et al. (2018) concluded that earlier estimates have been too high. Their own estimate is 17.4 million deaths.8
The global death rate of the Spanish flu
How do these estimates compare with the size of the world population at the time? How large was the share who died in the pandemic?
Estimates suggest that the world population in 1918 was 1.8 billion.
Based on this, the low estimate of 17.4 million deaths by Spreeuwenberg et al. (2018) implies that the Spanish flu killed almost 1% of the world population.9
The estimate of 50 million deaths published by Johnson and Mueller implies that the Spanish flu killed 2.7% of the world population. And if it was in fact higher – 100 million as these authors suggest – then the global death rate would have been 5.4%.10
The world population was growing by around 13 million every year in this period which suggests that the period of the Spanish flu was likely the last time in history when the world population was declining.11
Other large influenza pandemics
The Spanish flu pandemic was the largest, but not the only large recent influenza pandemic.
Two decades before the Spanish flu the Russian flu pandemic (1889-1894) is believed to have killed 1 million people.12
Estimates for the death toll of the “Asian Flu” (1957-1958) range from 1.7 to 2.7 million according to Spreeuwenberg et al. (2018).13
The same authors estimate that the “Hong Kong Flu” (1968-1969) killed between 2 and 3.8 million people.14
The “Russian Flu” pandemic of 1889-1890 is believed to be caused by an H3 pandemic virus.15 According to Spreeuwenberg et al. (2018) around 3.7 to 5.1 million people died worldwide.16
The “Swine flu” pandemic of 2009-2010 was caused by a new H1N1 pandemic virus. Several research groups have made estimates of the global death toll, which ranges from 130,000 to 1.87 million people worldwide.17
What becomes clear from this overview are two things: influenza pandemics are not rare, but the Spanish flu of 1918 was by far the most devastating influenza pandemic in recorded history.
This last visualization here shows the life expectancy in England and Wales by age.
The red line shows the life expectancy for a newborn, with the rainbow-colored lines above showing how long a person could expect to live once they had reached that given, older, age. The light green line, for example, represents the life expectancy for children who have reached age 10.
It shows that life expectancy increased at all ages, which means that the often-heard assertion that life expectancy ‘only’ increased because child mortality declined is not true.
With respect to the impact of the Spanish flu it is striking that the visualization shows that the pandemic had little impact on older people. While the life expectancy at birth and at young ages declined by more than ten years, the life expectancy of 60- and 70-year olds saw no change. This is at odds with what one would reasonably expect: older populations tend to be most vulnerable to influenza outbreaks and respiratory infections. If we look at mortality for both lower respiratory infections (pneumonia) and upper respiratory infections today, death rates are highest for those who are 70 years and older.
This data tells us that young people accounted for a large share of the deaths, this made this pandemic especially devastating.
Why were older people so resilient to the 1918 pandemic? The research literature suggests that this was the case because older people had lived through an earlier flu outbreak – the already discussed ‘Russian flu pandemic’ of 1889–90 – which gave those who lived through it some immunity for the later outbreak of the Spanish flu.18
The earlier 1889-90 pandemic might have given the older population some immunity, but was a destructive event in itself. According to Smith 132,000 people died in England, Wales, and Ireland alone.19
Writing in early March 2020 it is an obvious question to ask how the ongoing outbreak of Covid-19 compares. There are a number of important differences that should be considered.
They are not the same disease and the virus causing these diseases are very different. The virus that causes Covid-19 is a coronavirus, not an influenza virus that caused the Spanish flu and the other influenza pandemics listed above.
The age-specific mortality seems to be very different. As we’ve seen above, the Spanish flu in 1918 was especially dangerous to infants and younger people. The new coronavirus that causes Covid-19 appears to be most lethal to the elderly, based on early evidence in China.20
We’ve also seen above that during the Spanish flu many countries tried to suppress any information about the influenza outbreak. Today the sharing of data, research, and news is certainly not perfect, but very different and much more open than in the past.
But it is true that the world today is much better connected. In 1918 it was railroads and steamships that connected the world. Today planes can carry people and viruses to many corners of the world in a very short time.
Differences in health systems and infrastructure also matter. The Spanish flu hit the world in the days before antibiotics were invented; and many deaths, perhaps most, were not caused by the influenza virus itself, but by secondary bacterial infections. Morens et al (2008) found that during the Spanish flu “the majority of deaths … likely resulted directly from secondary bacterial pneumonia caused by common upper respiratory–tract bacteria.”21
And not just health systems were different, but also the health and living conditions of the global population. The 1918 flu hit a world population of which a very large share was extremely poor – large shares of the population were undernourished, in most parts of the world the populations lived in very poor health, and overcrowding, poor sanitation and low hygiene standards were common. Additionally the populations in many parts of the world were weakened by a global war. Public resources were small and many countries had just spent large shares of their resources on the war.
While most of the world is much richer and healthier now, the concern today too is that it is the poorest people that are going to be hit hardest by the Covid-19 outbreak.22
These differences suggest that one should be cautious in drawing lessons from the outbreak a century ago.
But the Spanish flu reminds us just how large the impact of a pandemic can be, even in countries that had already been successful in improving population health. A new pathogen can cause terrible devastation and lead to the death of millions. For this reason the Spanish flu has been cited as a warning and as a motivation to prepare well for large pandemic outbreaks, which have been considered likely by many researchers.23